
"A curse from the gods": India's tuberculosis crisis
Manoj Kumar sat, emaciated, on a hospital bed, with a black scarf over his mouth. His legs were nearly as thin as his arms and he could no longer walk. “Everyone used to come close to me,” he said. “They loved me. But now no one cares about me. I feel so helpless.”
Last year Manoj, who is 36, came down with a persistent fever and cough. Then blood started appearing when he went to the toilet. He was diagnosed with tuberculosis (TB), a bacterial disease which slowly devastates the lungs and other parts of the body, killing the patient unless they receive treatment.
Manoj is one of many Indian citizens coping with this terrible disease. India has the highest burden of both TB and drug resistant TB in the world, with 2.7 million of the world’s 10 million people diagnosed with the disease in 2017. Some 135,000 had the drug resistant form, a quarter of the world’s total. India, and other poorer countries, are struggling to cope as the drug resistant forms of TB create new challenges.
In Victorian times, authors such as Charles Dickens wrote movingly about what they then called consumption which was a major killer in the West until the invention of antibiotics 70 years ago. It is still rife in India in both its traditional and now drug resistant forms.
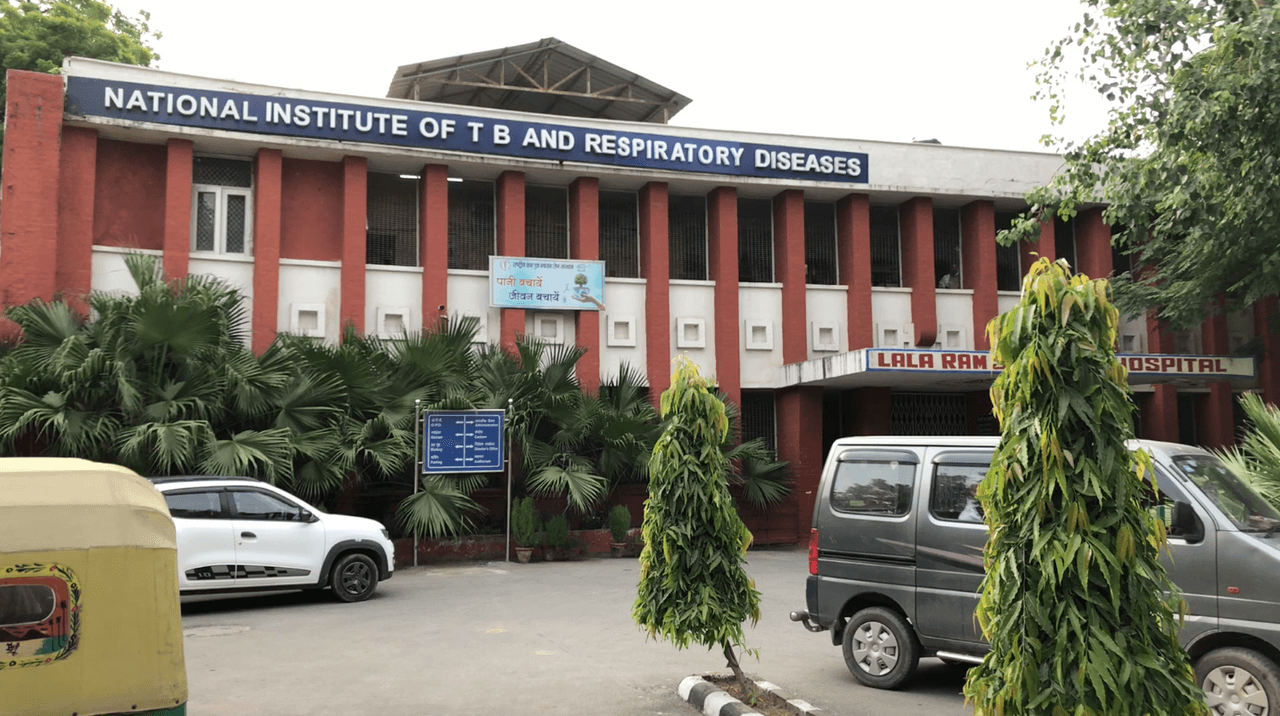
Manoj was told he had the multidrug resistant (MDR) form of the disease, meaning it would not respond to two of the most powerful anti-TB medications. It would take two years to treat, using drugs with potential side effects including deafness, psychosis and seizures. He came to the National Institute of Tuberculosis and Respiratory Diseases (NITRD) in Delhi, one of the top government TB hospitals in India, to be put on treatment. He received antibiotics for four months but saw no improvement. He has been back at the hospital for two months receiving a different mix of drugs: 10 tablets and one injection every day.
Manoj is originally from Ghaziabad, a city 35 km from Delhi, in the northern Indian state of Uttar Pradesh. He lives there with his wife and 11-year-old son in a single room, close to his mother and two brothers. Since he was diagnosed with TB most family members have refused to visit him, and he has become depressed. “I feel so lonely now...I feel like committing suicide at times,” he said. He has suicidal thoughts a lot, especially when he calls his family members to ask them to visit him and most don’t come. Negative thoughts are a known side effect of MDR TB medication but Manoj has not received any counselling.
His family fear they will catch TB from him if they visit. He said this is why TB patients often keep their disease a secret from their community. “They are not comfortable because everyone else starts discriminating against them,” he said “Other people feel scared that they might get TB from the TB patient.”
Tackling TB in India
The fear of infection is not unfounded - while there are only around 5,000 cases of TB in the UK a year, around the world it is the single biggest infectious killer, outranking HIV. This is despite the fact that it is completely curable with timely diagnosis and treatment.
Within the country more than 420,000 TB patients, some also with HIV, died in 2017, a figure higher than the population of Cardiff. It is thought there are are more between one and five million ‘missing’ patients going unreported. Those who are undiagnosed or receiving lower quality treatment are more likely to transmit the killer disease to other people.
Despite these multiple challenges, the Indian government has ambitious plans to eliminate TB by 2025, ten years earlier than the World Health Organisation’s (WHO) global deadline. However, doctors, NGOs, survivors and advocates warn that India almost certainly will not meet the target because of a lack of disease prevention, delays in correctly diagnosing patients, inadequate treatment and the growing epidemic of drug resistant TB.
The Bureau newsletter
Subscribe to the Bureau newsletter, and hear when our next story breaks.
The Bureau travelled to India to learn about the devastating issues faced by MDR TB patients and to witness in practice how the national TB control programme is working to eliminate the disease within seven years. We visited hospitals, treatment centres, patient support groups and patients living in the slums of Delhi.
“India has done a lot of politicking and they know the right words to say but they haven’t been brave enough, I think, to look their epidemic in the face and try to do the things we know work,” said Dr Jennifer Furin, Lecturer on Global Health and Social Medicine at Harvard Medical School and practising doctor.
The Bureau asked the Indian government's TB control programme for a comment but it did not respond by the time of publication.
What is TB?
TB is an infectious airborne disease caused by Mycobacterium tuberculosis. Typically, it affects the lungs but it can also affect other parts of the body like the gut and spine. Symptoms include coughing (sometimes with blood), high fever, fatigue, weakness, weight loss and infertility in women.
It is spread by people with the infection coughing, sneezing, breathing or speaking, especially in crowded or poorly ventilated areas like hospitals, prisons and slums. Around 40% of people in India, a higher proportion than elsewhere in the world, carry the bacteria. This is known as having latent TB, and only one in ten will go on to develop the disease. People with HIV are much more vulnerable to TB: there are 86,000 people in India who have both HIV and TB. India’s high rate of diabetes also exacerbates the problem as diabetics are also more prone to TB. Breathing in pollution, and heavy smoking or alcohol habits also increase the risk of the disease.
There are currently no vaccines to prevent TB in adults, though there are 12 currently in clinical trials. The bacille Calmette-Guérin (BCG) vaccine is administered to children in India, but only prevents severe forms of TB. It is less effective against respiratory TB, the most common form of TB in adults.
A disease of poverty
While TB affects everyone, it is widely known as a disease of poverty. The poorer the community, the greater the likelihood of people becoming infected and developing disease. More than 13% of people in India live in poverty, according to the World Bank's latest figures, from 2015.
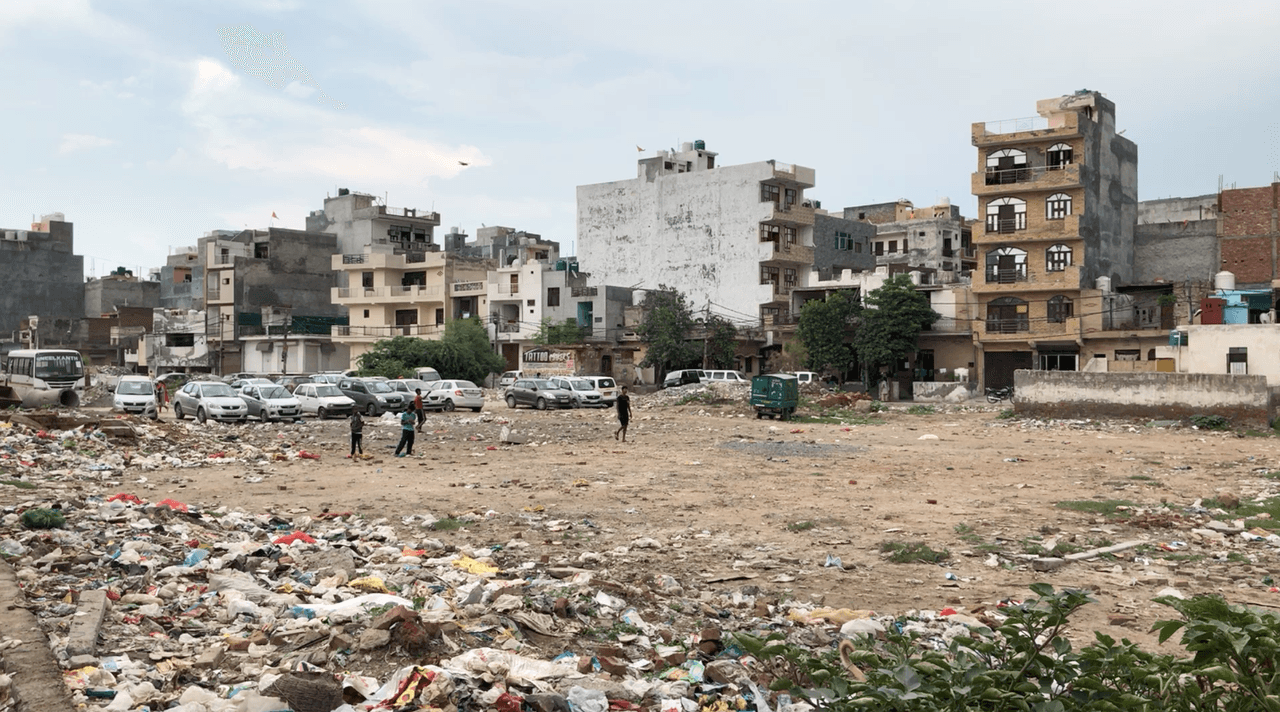
East of Delhi, beyond an abandoned coal power station, is an urban slum known as Burari. There, 1.5 million people live in just 11 square kilometres. The buildings there are unauthorised and, as such, the government does not provide basic services like electricity.
There are open drains, which flood the narrow roads with sewage when it rains. Children run through the foul-smelling water barefoot. The drinking water comes from hand pumped boreholes. There are crumbled buildings, bogs covered in green slime (pictured below) and rubbish piles everywhere, with children scavenging or flying kites on them. Dogs line the streets. In some areas there are outbreaks of dengue, malaria and Chikungunya, a viral disease. TB is also rife, as the bacteria proliferate in the dank, dark conditions.
The people living here are poor; many are migrant workers and labourers, eking out an existence on a daily wage. People living in such areas tend to be malnourished which lowers their immune system and makes them more susceptible to TB. Many live in crowded houses, with whole families living in one room, so families are more likely to catch the disease from an infected member.
In one part of the slum two or three members of every family are being treated for TB, said Jyoti Gupta, a counsellor with a non-governmental organisation (NGO), TB Alert India, which runs TB services in this area as the government does not run clinics here. Instead, healthcare is provided by nine qualified private doctors, 130 informal providers (called quack doctors by critics) and NGOs.
There can be a lack of education around symptoms of illness in poor communities like Burari. Factors such as the cost of travel, fear they will lose out on their daily income or the perception doctors might look down on them all mean that people in poor communities can be less likely to seek healthcare. Without access to good quality healthcare there are longer delays between diagnosis and cure. This, in turn, perpetuates the spread of TB.
TB Alert India stepped in to provide TB services in the Burari slum in 2008, and diagnosed 300 patients within the first year. Now, some 11,500 patients a year are found and diagnosed. The NGO runs five clinics where people are screened for TB, tested for HIV and diabetes, and where diagnosed patients pick up their medicines daily.
 A large expanse of polluted waste-water on the outskirts of Delhi
A large expanse of polluted waste-water on the outskirts of Delhi
 Children playing barefoot in dirty water in the Burari district of Delhi
Children playing barefoot in dirty water in the Burari district of Delhi
There are thousands of slums like Burari in poor and densely populated areas of cities all across India, where TB is rife. In a city like Mumbai, 3% of the population has TB and it is one of the leading causes of death, disability and unemployment. “We can’t just address TB as a disease with drugs, but also the other social issues: housing, food, out of pocket expenses,” said Blessina Kumar, CEO of the Global Coalition of TB Activists and a TB survivor herself. She added: “The populations that get TB are the most vulnerable and the most marginalised.”
The NGO faces many logistical problems common in TB clinics. Staff report delays in patients receiving their diagnosis from the local hospital and delays in obtaining key lab equipment. The government does provide free TB drugs, but they often arrive late, sometimes with only a few weeks before they are due to expire. Sometimes only drugs for TB patients, not those with drug resistant strains, arrive.
“The delay in medicine supply creates a problem for the patients,” said Shobha, a lab technician at TB Alert India. “The patient has to make do with half their dose. Sometimes they are told to make do without any medicines.” Missed or half doses are a primary cause of the development of more resistant forms of the disease.

Curing TB - a long, hard haul
The cure for TB is long and difficult, involving six months of taking a cocktail of four drugs with undesirable side effects, and a 20% chance of the disease returning. But whereas combating TB is well understood, new strains are challenging overburdened health systems in poorer countries.
Now, drug resistant, strains have become common in India, and the country is struggling to cope. These strains can take between nine months and two years to treat. The drugs for these carry even more severe side effects. Only one in two Indians recover from multi drug resistant (MDR) TB and only one in three make it if they have extensively drug resistant (XDR) TB. “It’s absolutely unacceptable,” said Dr Furin.
Drug resistance develops when patients with TB are mismanaged. People with TB are given a strict six-month regimen of four drugs and attend a clinic every day so a health worker can check they have taken their medicines. If people with TB are given inappropropriate or ineffective drugs, resistance can evolve. Patients might be treated with a single antibiotic rather than the recommended cocktail, or the drugs might be of poor quality or kept in bad storage conditions.
If the patient doesn’t take their medicine every day for the full course, they can develop drug resistance. Drug resistant TB can then be transmitted in the same way as classic TB, from person to person, especially in crowded places like prisons, hospitals and slums.
The drugs used to treat drug resistant TB can trigger severe side effects. For example, between 40% and 60% of people put on them go deaf. Dr Furin said she has to tell her patients: “It’s better to lose your hearing than to die”.
The main TB antibiotic, rifampicin, turns the body’s secretions red. Other side effects of TB drugs include gastrointestinal problems, dizziness, vomiting, skin discolouration, hepatitis, nerve damage (causing weakness, numbness and pain), an under-active thyroid and epileptic seizures. One of the medications, cycloserine, can also trigger depression, anxiety and psychosis.
Patients are often not told about these side effects because doctors in government hospitals are overburdened and don’t have time to counsel patients. Nandita Venkatesan, 26, survived an eight year battle with a rare form of intestinal TB. She has since become a TB advocate and mentor. She was given kanamycin injections to treat her TB, and lost her hearing as a result.
She was not told about this side effect, so the experience was all the more traumatic. “The hearing loss was catastrophic to say the least,” she said. She was not forewarned, she added. “So I slipped into a very long period of depression.”
A combination of many factors, including the awful side effects of medications, the inconvenience of treatment, lack of education and people migrating to different parts of the country for work or family commitments means many patients stop taking their medicine. Others die before completing treatment.
The system is so disruptive for patients that many stop taking their medicines once they feel better, said Dr Batra. Government healthcare facilities are only open from 8am-4pm. She added: “If a man is a daily wage labourer is he going to work or is he going to go for his TB treatment?...He might go for one, two days a week, he can’t go for six months. Typically when patients start feeling better they drop out, and that’s how drug resistant TB sets in.”
The NGO, Operation Asha, has devised systems to keep patients taking their medications, Dr Batra said. It has started running clinics in places more convenient for patients: temples and mosques, as well as community centres. It also uses eye scanners and fingerprint scanners to identify patients when they come to take their medicines, so staff are absolutely sure that patients have taken their pills. Notifications are sent back to the office in real time.
If a patient doesn’t turn up, an Operation Asha health worker visits their house that day to support them, give them medication and find out why they have not attended.
However, there is currently little to no follow up of patients in government hospitals or community clinics once they are discharged, or if they stop turning up to take their medicine. Patients drop out at every level. Some 18% of drug resistant TB patients are lost after diagnosis. “Nobody knows and nobody cares,” Dr Batra said.

Cursed - how TB still carries stigma
One of the biggest barriers to elimination in India, is that the condition is still seen as shameful, according to Dr Batra. “TB has been regarded as a curse from the gods, or for your past karma, anything except a curable infectious disease,” she said. “Stigma is a very big issue is and still is. [Patients say] ‘my husband will know, my neighbours will know, my landlord will know and I’ll be thrown off my patch of land where I’ve made my hut.’”
Women who suffer TB are regularly divorced, or fear for their future marriage prospects. Around 100,000 women a year are abandoned by their families to die of disease and starvation because they have TB, according to a 2008 government report. Ms Venketasan said she was recently contacted by a man whose family was pressuring him to leave his wife as she had TB. “I was telling him ‘don’t do this. This is the time your wife needs you and she needs your support,’” she said.
The same report said 300,000 children are forced to leave school every year because of TB. “Either they are too sick, the school authorities don’t want them, or the wage earning parent is sick and they have to take up a job,” Dr Batra said.
Manoj Kumar, for his part, claims his son has been thrown out of school due to his father’s TB diagnosis. “His name was struck off from the school roll by the principal,” Manoj said. “They feel that since I have this disease my son might be a carrier, and through him other children might get the disease...it makes me feel very helpless to think about how I am able to do nothing for my son and how he is suffering because of my disease,” he added.
Both Dr Batra and Ms Venketasan believe counselling for patients to start treatment, to keep taking their medicines, to deal with any side effects and to combat shame is the only way India will eliminate TB. Having people go to patients’ homes and explain to their whole families the importance of taking the medications, of good nutrition and to talk about any side effects they might be experiencing is very effective and means fewer patients stop treatment, they said. “If I had been given proper counselling I would have faced fewer problems than I had to face,” Ms Venketasan said. Currently the government relies on NGOs like Operation Asha and TB Alert India to counsel patients.
Some people believe the word ‘stigma’ in itself is problematic. “We use the word stigma but what these people face is frank discrimination,” said Dr Jennifer Furin. “If you’re going to be beaten up and kicked out of your house that’s not stigma, it's violence and discrimination. If you’re fired from your job because you have MDR TB, that’s discrimination,” she said.
Patients also put pressure on themselves. Ms Venketasan talks of what she calls ‘self-stigma’, where patients begin to feel ashamed of themselves, that it is their own fault they have the disease. “There is a deep silence about this illness,” she said. “All this compounds into self-stigma, which is very high. You start thinking, ‘Is it my crime that I got this illness?’”
As a result, suicidal tendencies are very common, though there is a paucity of research on this. One small study looking at suicide in TB patients in South Africa found 9% of patients had suicidal thoughts, and 3% had a history of suicide attempts. “That was the case with me myself,” said Ms Venketasan. “I was in a very late phase of depression, I had all the wrong thoughts of giving up more than once.”
Diagnosing TB
One of the most important pillars of eliminating TB is timely diagnosis, as each undiagnosed patient can transmit the disease to others. A study by the Global Coalition of TB Activists found it took between a month and more than two years for patients to get a proper diagnosis. “That’s the most dangerous time in terms of transmission,” said Blessina Kumar, CEO of the Global Coalition of TB Activists.
Here, too, doctors think that the stigma of TB has led to some patients being reluctant to be screened. “First of all a patient would be in denial. ‘I don’t have TB, I can’t have TB, my son can’t have TB. We are a better class than the neighbours so how can we get TB.’ All these things will be there in their minds.” said Dr Batra.
Some 70% of people in India also visit private doctors or people practicing alternative systems of medicine, called quack doctors by critics, for their treatment. Not all are attuned to diagnosing TB, or know the correct cocktail of drugs to prescribe for patients.
Private doctors should notify the government when a TB diagnosis is made, and now receive an incentive of 500 rupees (£5.45) when they do so. But it is still not always done. In 2017 just over 400,000 notifications were made from the private sector, compared to more than 1.5m from the public sector.
Varun Kumar, 22, told the Bureau that it took two months for him to diagnosed with MDR TB at a private hospital. During that time he received hospital visits from his two brothers. His younger brother Shivam also became infected and then died, also in a private hospital. “They did not provide proper treatment,” Varun said. “By the time my brother was brought to the government hospital for treatment it was too late. He was admitted for six to seven days after which he passed away.”
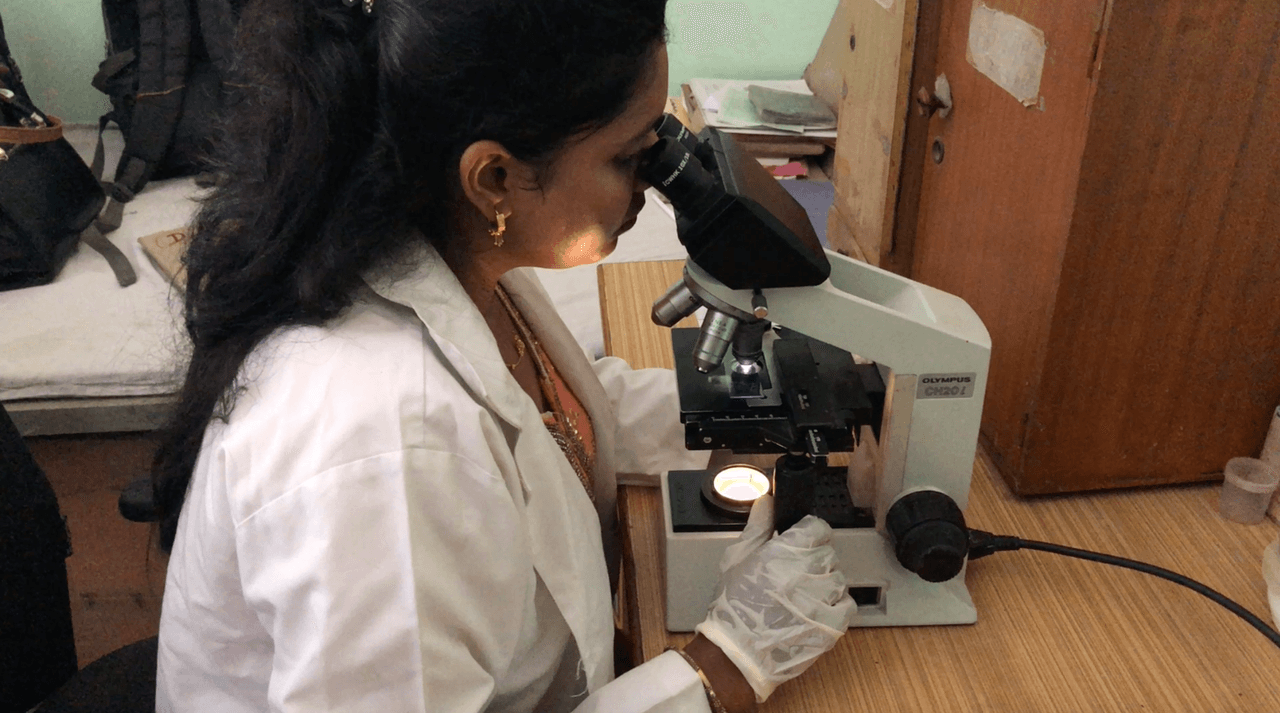
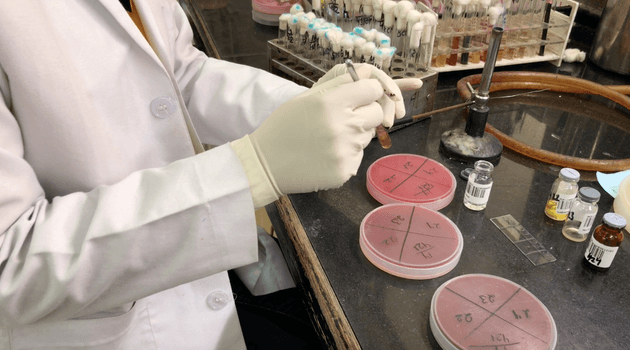
Even if patients reach a competent doctor, TB is difficult to diagnose as the symptoms can be similar to viral illnesses, pneumonia or bronchitis. The method most commonly used to diagnose TB in India, is sputum smear microscopy, where a patient’s phlegm is smeared on a glass slide and examined under a microscope. It is widely used because it is inexpensive and straightforward. It doesn’t require a laboratory so it can be done in community centres. But it is insensitive: it misses up to half of cases. “We are using sputum smear tests, a test that is over a 100 years old. Why are people being given tests that are not accurate?,” said Blessina Kumar.
 Health-care staff examining specimens for diagnosis
Health-care staff examining specimens for diagnosis
She and others believe sputum smear tests should be replaced by a faster and more accurate molecular test, called GeneXpert or CBNAAT. CBNAAT is highly sensitive, takes only two hours to produce a result, and tells doctors the patient has a drug resistant form of the disease. However, in reality, obtaining results takes longer in busy hospitals, being dependent on staffing. TB Alert India staff in the Burari centre said tests could take 10 days to come back. The machines are expensive, with units costing $17,000 and each individual test costing nearly $10. It also requires a constant electricity supply and air conditioning, which is not always easy to obtain in poor or rural areas.
There are currently 1,135 CBNAAT machines across the whole of India, which is divided into 644 districts. However, there are many remote areas too far from a CBNAAT machine for it to be used routinely. Ms Kumar pointed to better practice elsewhere. “In South Africa the moment the CBNAAT machines came out, the prime minister, he just ordered thousands.”
After a CBNAAT test, in order to tell which strain of MDR or XDR TB the patient has and which customised cocktail of drugs will work best to cure their infection, further tests called ‘drug susceptibility tests’ need to be done in a laboratory, which can take several weeks. This is crucial as without it the patients can be put on the wrong regimen of drugs, which means their disease is not being cured and fuels resistance.
While 2017 Indian government guidelines advise carrying them out, they are not always done. In 2015 only a quarter of patients were offered the tests, according to the government’s own report. Drug susceptibility testing "is just not happening today,” Ms Venkatesan said. “Even if the government claims it is happening, it is not. I know of people who have been diagnosed almost six months to a year late, and a year is too long a time to be lost and you’ll end up becoming resistant to more drugs in this time. And that’s because the drug susceptibility tests were not done.”
 Shakuntala, who has extensively drug resistant TB, speaks about her experience
Shakuntala, who has extensively drug resistant TB, speaks about her experience
XDR TB: Shakuntala’s story
Along her neck, 26-year-old Shakuntala has a series of puckered scars where her brown skin is twisted and shiny. In 2015 she was working as a nursery school teacher, but she soon became so ill that she couldn’t work.
She had a fever, and lost her appetite. Then she got swellings and knots in her throat that were very painful. She went to the doctor but blood tests carried out came back normal. It was only after they tested the fluid from the swellings that they diagnosed her with tuberculosis (TB) in May. Her brother had previously suffered the disease and she may have caught it from him.
After six months of treatment with four antibiotics, it was found she had MDR TB, and in multiple organs, including her abdomen lymph nodes, which is why there were swellings on her neck. She had her lymph nodes removed, which left her with a series of scars.
From 2016 to 2017 she began treatment with a different regimen of drugs. The injections she had to take caused headaches and dizziness. “My entire body temperature used to rise and that would make my temper very sour,” she said.
As the end of her treatment was near and she began to look for a job. People asked her about the marks on her neck, asking her if she had a disease, or if she had been burnt. She told them about her TB and was rejected from many jobs. “I did not feel bad when people would ask me about it,” she said. “But I was really hurt when people started declining jobs to me because of these marks as I know that I was capable of doing those jobs."
When she did eventually find a job, she fell ill again. She was admitted to hospital and it was found pus had accumulated in her liver. Just when she thought she was going to be cured, tests showed she had XDR TB, which has such a bad prognosis many consider it a death sentence. She had heard XDR TB can lead to blindness, and felt worried. She said she cried a lot that day.
This time the medicines turned her complexion dark red, and she felt a strange sensation in her legs. Last November she was admitted to hospital again as she was vomiting and couldn’t digest anything she ate. She was so weak she could barely walk. “I wanted to die,” she said. “That was a very low point for me.” At the hospital they gave her a blood transfusion. Since then her health has improved.
Her father, who sells lemons at a market in Azadpur Mandi, Asia’s biggest fruit and vegetable market in Delhi, has been supporting her throughout her treatment. “Come what may, he always finds a way to bear the financial responsibilities of my treatment and health,” she said.
Most of her friends are now married, so no longer live in Burari. Shakuntulah said she hopes to get married when she becomes healthy again. “I wish for a boy who does not stop me from doing anything. And who accepts me despite my having suffered from this disease.”

The poorest shoulder the heavy costs of TB
Back in Ghaziabad Manoj had a job selling momos, Indian dumplings, from a cart. When he was diagnosed with TB he had to quit his job, and his family are now suffering financially. His wife has taken out loans to support Manoj staying in Delhi for treatment. “I want to work but I am so weak that I cannot” he said. The family is unable to give their son everything that he needs.
This story is common; families where a member has TB will lose 30-60% of their income. “People are thrown out of jobs, entire families sink into poverty,” said Dr Batra. “The loss of wages alone in a country alone is up to $300m [£230m] annually.”
The government’s elimination strategy for TB does focus on reducing the catastrophic costs of TB, as does WHO's End TB strategy. In April 2018 the Indian government introduced a subsidy of 500 rupees a month to every TB patient so they can buy the food they need, as nutrition is so important in fighting the disease. However, only newly diagnosed patients can currently claim the subsidy. Patients also need a bank account and an Aadhaar number, a 12-digit identification number given to each citizen, a recent government initiative that is controversial; there is an ongoing court case about whether it breaches the right to privacy.
The Bureau asked the Central TB Division in India how many people had received the subsidy since April but it did not respond. Reports in the Indian press said only 12% of eligible patients had received it, two months after it was announced.

Searching for the missing cases
Currently if a patient has TB or MDR TB, their family should all be tested for the disease, according to WHO guidelines. In slum areas where TB is rife, there should be health workers going into the slums to find families with TB, a process known as ‘active case finding’.
The Indian government says it is ramping up active case finding in order to find more missing cases, though it did not respond to the Bureau’s request for how many patients it had found already through this process. In Delhi state, Dr KK Chopra carried out programmes to find patients in vulnerable groups: sex workers in brothels and drug addicts. They discreetly found and treated around 70 people. Next he plans to test prisoners in the Tihar jail, which houses 15,000 inmates in cramped conditions. “Their nutritional conditions and their general behaviour are like that they are vulnerable to TB. So we will be doing daily investigations there,” he said.
Children whose family members have TB, especially drug resistant forms, should be given antibiotics to prevent them getting the disease. However, only 11% of eligible children receive this preventative therapy, according to WHO.
Dr Furin fears without measures such as these being urgently scaled up in India, the government’s promises of elimination are simply rhetoric. “MDR TB is largely driven by person to person transmission,” she said. “We have to find people quickly, they need drug susceptibility testing quickly and they need to started on the best regimens possible as quickly as possible. Along with preventative therapy for people who have been exposed. That’s the only way it’s going to stop. But nobody’s going to do that under the current Indian administration.”
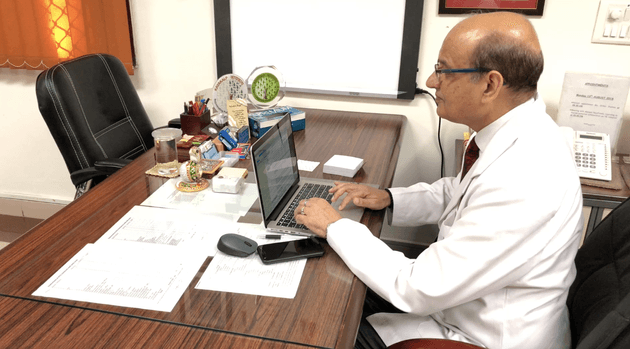 Dr Rohit Sarin reads a letter from a patient cured of drug resistant TB by new medication
Dr Rohit Sarin reads a letter from a patient cured of drug resistant TB by new medication
Rationing new drugs
At the National Institute of Tuberculosis and Respiratory Diseases (NITRD), Dr Rohit Sarin, the hospital’s director, adjusted his glasses and read out a letter from a patient who received bedaquiline, one of the first drugs for MDR TB to be developed in 50 years.
“Honourable sir, it is indeed a big day for me and my family,” Dr Sarin read. “You have not just given me a new life, instead you have given me a new hope, a new beginning, a new vision for my life.”
This patient was one of less than 2,000 who has received bedaquiline, an oral drug which has been recommended by the WHO to replace the injectable antibiotics taken by MDR sufferers. There was initial caution over the antibiotic because trials showed higher mortality in groups that received it (though this was not found to be attributable to the drug). The WHO recommended it in August 2018 after new research was published, including a South African study which found treatment regimens which included bedaquiline reduced MDR TB deaths by two thirds.
In South Africa, where there are 14,000 people with MDR TB, around a tenth of the number of such patients in India, the drug has already been given to 11,000 people. Less than 2,000 have received it in India, despite it being donated by its manufacturer. The government restricted its use to six government hospitals, fearing if it was more widely available it would be overused and resistance would develop.
The drug is now only given as a last resort in few hospitals such as NITRD where it is available, and a lengthy process must be followed to receive it, including a long ‘informed consent’ form. Campaigners say this rules out uneducated, illiterate people who might need it. “There’s all kinds of barriers put up,’ explained Dr Furin. “And desperate people go to those hospitals but they still don’t get the drug.” In 2017 18-year-old Shreya Tripathi, who has XDR TB, successfully won a court case in order to access bedaquiline at a private hospital in Mumbai, paving the way for similar legal actions from other patients.
There are many who agree with the government’s view. Dr Jay Desai, of the Children's Hospital Los Angeles, said those who think use of bedaquiline will solve the TB crisis are “barking up the wrong tree”. “How does resistance develop?,” he said. “Because of lack of compliance. Bedaquiline is very important in the battle against TB but what makes us think people are going to be compliant with it?”
Dr Furin believes fears of future resistance should not trump saving dying patient’s lives. “Here you have a country standing up and claiming they are going to eliminate TB by 2025, that's seven years from now. Yet they ration access to one of the best drugs we have,” said Dr Furin. “TB elimination doesn’t look like that, it’s not what it looks like.”

Missing India's target
In order to eliminate TB, the number of new cases will need to be reduced by more than 10-15% every year, the government admits. It is currently decreasing at around 2% a year - but the cases of MDR and XDR TB continue to rise.
In 2018 the Indian government increased the budget for TB to $580 million, funding 79% of this itself. But experts question if this is enough when the country spends less than 4% of its GDP on public health including the private sector, one of the lowest proportions in the world, and a quarter of its urban population still lives in slums.
Experts disagree on whether preventing the disease in the first place, improving housing, improving nutrition, reducing the shame of the condition, facilitating better diagnosis, convincing patients to keep taking their medicines, better access to new drugs or developing a TB vaccine are the most important factors to achieve the target.
If India can challenge the spread of the disease, more Indians will not have to suffer years of painful treatment, like that suffered by Manoj Kumar. He has lost hope in the future. ‘I am not even sure whether they will be able to treat me successfully or not,’ he said. ‘I do not feel sure whether I will survive or not. I feel very weak even now.’ He said if he does recover he would like his son to return to school, and he would like to go back to work to secure a future for his family.
He remembers what life was like before the condition took hold. “I was healthy and could work then,” he said. “All my family and friends were close to me at that time. Now no one likes to come near me.”
Header picture of Manoj Kumar. All pictures by Madlen Davies/the Bureau. Contact us for re-use. Translating by Mansi Sharma.





